Knee
Select a treatment from the list below.
Performed by – Alastair Davidson, Azal Jalgaonkar, Richard Hargrove, Jonathan Hull, Zuhair Nawaz Andrew Perry, Seb Sturridge, James Singleton
Knee arthroscopy is commonly known as keyhole surgery. It involves a camera attached to a thin telescope that is inserted into the knee via a small incision of less than 1cm. With the camera, the surgeon can look inside the knee itself and identify any problems. If the camera reveals any problems the surgeon can use small instruments that can be inserted via a second small incision in the knee. Common problems that are treated by arthroscopic surgery include meniscal cartilage tears, worn articular cartilage and problems with the soft tissues within the knee joint such as synovial plicas. In addition, complex surgery such as cruciate ligament reconstruction can be performed using keyhole surgery techniques.
What happens in surgery?
The surgery is generally performed as a day case under a general anaesthetic. The operation usually takes around half an hour to perform although the time taken may be longer for more complex procedures. At the end of the operation your knee is injected with a local anaesthetic to minimise the post-operative pain.
Arthroscopic Meniscectomy & Meniscal repair
Meniscectomy involves trimming a torn cartilage using special keyhole surgical instruments. The meniscus is a crescent shaped rim of cartilage between the femur (thigh bone) and tibia (shin bone). If it is torn, it can catch in the knee causing pain. Only the torn part is removed, leaving the remaining uninjured cartilage behind. Arthroscopic meniscectomy has a high rate of success providing relief from knee pain. Where possible the meniscus is repaired using internal stitches, unfortunately this is the minority of cases and the failure of such repairs is one in four as the cartilage heals poorly.
Arthroscopic Microfracture & Chondroplasty
Damaged articular cartilage on the ends of the bones has very poor healing potential. Flaps of worn articular cartilage can catch as the knee moves and create pain and discomfort. ‘Chondroplasty’ involves trimming and smoothing these areas of cartilage, and so pain and mobility can be improved. Where there is a full thickness defect ‘microfracture’ may be beneficial which involves making small holes into the bone to release bone marrow cells and bleeding to promote healing which otherwise would not happen. It is important to recognise that worn articular cartilage is, potentially, the start of osteoarthritis in the knee and that your knee will not be returned to complete normality after this surgery.
Arthroscopic Soft Tissue Debridement
Sometimes folds of tissue in the lining of the knee can catch and become inflamed. These tissue folds are called plica. Not everybody has them and, even if you do, they may not be symptomatic. However, a plica may cause pain on the inside of the knee and around the patella. The plica can be trimmed with a small arthroscopic shaver and the symptoms relieved.
What happens after surgery?
You will be mobilised after surgery by a physiotherapist and will be able to walk out of the hospital a few hours after the surgery, although unable to drive for a few days or few weeks depending on surgery and leg involved. You will need to have outpatient physiotherapy for a few weeks after your operation to get your knee to settle and move as quickly as possible. Your mobility will improve each day after surgery. You will need a week or two off work depending on your job and the exact nature of the surgery. Your knee should be back to normal by 2-3 months depending on exactly what has had to be done.
Performed by – Alastair Davidson, Jonathan Hull, Zuhair Nawaz Andrew Perry, James Singleton
The ACL (Anterior Cruciate Ligament) sits in the middle of the knee linking the tibia (shin bone) to the femur (thigh bone) and is important in controlling movement of the two bones, particularly during twisting pivoting sports and dancing.
Anterior Cruciate Ligament Tear
The anterior cruciate ligament is commonly ruptured by twisting injuries such as a bad tackle in football or a fall whilst skiing. Typically, the knee will ‘give way’ and there may be a painful ‘popping’ sensation. You may even find that you are not able to get up and walk. Typically, your knee will swell over the next hour as the ruptured ends of the ligament bleed into the knee. If nothing is done the knee will slowly settle over six weeks but if you return to sport, you may suffer ‘giving way’ episodes similar to your initial injury when you twist and turn. If things are bad you may experience such instability on normal day to day activities.
Diagnosis of ACL Injury
The diagnosis depends on a clinical examination at which time the laxity of the ligament can be assessed to see if the cartilages are also damaged. It is often very difficult to examine a knee soon after the initial injury as it is swollen and painful. In this case it is usual to arrange for an MRI scan to confirm the diagnosis and physiotherapy to mobilise the knee and and help it recover. After a few weeks it is easier to examine the knee and to confirm the diagnosis.
Non-Operative Management
It is possible to rehabilitate your knee and get it working well after injury by a course of physiotherapy. This aims to strengthen the muscles around the knee to stop it giving way. If your sporting desires are not high it may be possible to avoid surgery, but there is an increased risk of further injury as the knee can ‘give way’ and you may fall because of it. If you wish to get back to running twisting sports physiotherapy is unlikely to make your knee stable enough and surgery is usually considered.
Operative management
Anterior cruciate ligament (ACL) reconstruction surgery is an arthroscopic (keyhole) surgical procedure. The same two small incisions as for arthroscopy are used at the front of the knee, with another small incision above the knee, and a 3-5cm incision at the front of the knee to obtain the graft and feed it into the knee. By operating with this technique we can perform this surgery as day case surgery under a general anaesthetic with a more rapid return to normal daily activities.
Anterior Cruciate Ligament Graft
The procedure involves excising the damaged ACL and replacing it with a graft of your own tissues. The surgeons at Joint Reaction recommend using a hamstring graft. In this technique tendons from the inside of your knee are removed via a 3-5cm incision just below the knee and used to reconstruct your ACL. Despite the loss of these tendons you are unlikely to notice a significant reduction in the strength of your hamstrings.
The graft is threaded across the knee via 2 drill holes. The first drill hole enters the knee where the ACL attaches to the tibia and the second is across the knee in the femur, where the ACL is also attached. Both of these drill holes are made through the small incision used to remove the hamstring tendons as the entry point is at the hamstring insertion on the tibia. The graft is pulled through the knee and fixed in place using special devices and screws.
Revision ACL Reconstruction
The surgeons at Joint Reaction have a large combined experience of this surgery due to treatment of a large population of sportsmen and women, as well as military personnel. Graft options used in revision cases will be discussed on an individual basis and may involve your own tissue or donor tissue ‘allografts’.
After surgery
Most ACL reconstructions are performed as a day case, but if the surgery is later in the day or if you live alone you may need to spend the night. The knee is filled with local anaesthetic at the end of the operation to numb the pain. You will be mobilised by a physiotherapist using crutches and given some exercises to perform. Your physiotherapy rehabilitation will start a week after surgery and is split into different phases. In the first 3 months you will regain a full range of movement mainly performing ‘closed chain exercises’. These are exercises with your foot on the floor or a pedal of a stationary bike that do not over stress the healing graft. After 3 months the graft has healed strongly to the bone in the tunnels either side of the knee joint and your rehabilitation can progress. Between 3 and 6 months you start ‘open chain exercises’ such as jogging in a straight line and progress to shuttle runs in the gym. You will also do ‘proprioception’ exercises to train the muscles to respond quickly. Between 6 and 9 months you can start sport specific training. If you want to play football you can return to training but should avoid tackling and competitive games. You can return to gentler sports such as tennis at this time.
Finally, at 9 months your rehabilitation is complete and you can return to your chosen sport although it is often sensible to avoid full competitive contact until one-year post surgery.
Success of ACL reconstruction
90% of patients should be able to get back to their chosen sport after an ACL reconstruction. However, some avoid it due to the risk of further injury to either or the same knee. The risk of ACL graft rupture is an approximately 6%, but it is this is also the risk of rupture of the normal ACL in the other knee.
Performed by – Alastair Davidson, Azal Jalgaonkar, Richard Hargrove, Jonathan Hull, Zuhair Nawaz Andrew Perry, Seb Sturridge James Singleton
Total knee replacement (TKR) is a surgical procedure in which injured or damaged sections of the knee joint are replaced with artificial parts. It is commonly performed for arthritis of the knee where the joint has become stiff and painful. Initially, Arthritis can be treated with painkillers, anti-inflammatories, physiotherapy and, in the earlier stages, arthroscopy (keyhole surgery) but as the knee progressively wears, joint replacement surgery may be required to relieve the pain and improve mobility.
What happens in surgery?
The surgery involves an incision over the front of the knee and through the quadriceps muscle. The surface of the joint is removed including a small thickness of the damaged bone ends of the knee, usually about a centimetre of bone is removed during the operation. The metal of the knee replacement fits on the cut ends of the bone and is fixed to the bone with cement, with plastic between. The operation takes about to an hour and a half.
Customised Knee Replacement.
There are many different types of knee replacement all of which the surgeons at Joint Reaction have experience in performing. Your surgeon will assess your knee and discuss the best option for you. One option, which is useful in some cases, utilises pre-operative scans to build customised cutting blocks to guide optimal knee replacement. This is not necessary in all cases but has some advantages.
The Component Parts of the TKR
The Total Knee Replacement comes in three parts. The femoral component is made of metal and is highly polished. The tibial component is made of metal with a curved plastic tray attached to its upper surface. This forms the new joint with the metal femoral component. The back of the patella is covered with a plastic button, which sits in a shallow groove on the front of the metal femoral component.
After a Total Knee Replacement
With the aid of a physiotherapist you will get out of bed and begin to exercise your new knee replacement. With perseverance, you should be able to climb stairs by day 3 and usually go home between day 3 and 5 depending on the speed of your recovery. Post-operative Physiotherapy, range of movement stretches and functional exercises are all very important to gain full function and range of movement of your TKR to get the best result of your TKR. You will need to continue attending physiotherapy as an outpatient. This can be done closer to your home with one of our recommended group of physiotherapists. For most people it will take around six weeks to be walking reasonably with only one stick and get back to driving a manual car, but three months to fully recover. It is important to remember that an artificial knee is not a normal knee. You should be able to carry out all normal activities of daily living, however the range of movement may not be as good as it was before surgery and you may be too uncomfortable to kneel after your knee replacement, although kneeling will not damage the knee. You should be able to get back to golf, gentle game of tennis, cycling, swimming.
Lifespan of the TKR
The majority of knees last ten to fifteen years with studies suggesting that a Total Knee Replacement in a 70-year-old has around a 94% probability of lasting for 10 years after surgery. If, however, the patient is younger and more active the replacement may not have such a high survival rate, in which case your surgeon will discuss other options with you.
Performed by – Alastair Davidson
Partial and Total Knee Replacements can now be performed using a computer guided robotic arm for assistance. The robotic arm acts as a guide to help the surgeon’s bone cutting precision, the surgeon still performs the procedure and inserts the implants. This is a useful technology to optimise results and outcomes. Joint Reaction surgeons have experience in performing this surgery and can discuss this technique with you to determine the best option for your knee replacement. This is not necessary in all cases but has some advantages. The knee replacement itself is a standard highly rated implant, it is the surgical technique that varies. If you opt for robotic assisted knee replacement you do not have to prepare or rehab afterwards in any different way from a conventional knee replacement and can fully weight bear after surgery.
Performed by – Alastair Davidson, Azal Jalgaonkar, Richard Hargrove, Zuhair Nawaz Andrew Perry, Seb Sturridge James Singleton
As arthritis deteriorates the pain can become debilitating and then surgery is considered. In some types of arthritis of the knee, only the medial (inside) part of the joint is affected. In this situation it is possible to replace the damaged part of the knee without resorting to a total knee replacement (TKR). This is called a unicompartmental knee replacement (UKR). The surgeons at Joint Reaction use the Oxford UKR which has the longest pedigree and best results. This preserves all the knees ligaments and thus mimics the function of a normal knee as best possible. The ‘Signature’ option is an MRI scan based technology that plans individualised surgical planning with customised cutting blocks.
What happens in Surgery?
The surgery involves removing a small thickness of damaged bone from the inside part of the knee. Less bone is removed than in a Total Knee Replacement and only from one side of the knee. The Unicompartmental Knee Replacement fits inside this prepared space. The Operation takes about an hour and involves a smaller surgical incision and a faster recovery. This is often described as ‘mini-invasive surgery’. This small incision does not involve cutting any muscle or tendons (as with a Total Knee Replacement), thus enabling quicker recovery from surgery.
The Component Parts of the UKR
The UKR comes in three parts. The femoral component is made of metal, is curved and highly polished. The tibial component is made of the same metal and has a flat upper surface. A plastic component, which is curved on the top and flat on the underside, sits on the flat tibial surface and can slide backwards and forwards. This mimics the meniscal cartilage in the normal knee. The upper part of this plastic insert articulates with the femoral component. This type of knee replacement is called a meniscal bearing and has the advantage of sharing the load through the knee over a large surface area, which helps to reduce wear and hence make the knee replacement last longer.
After a Unicompartmental Knee Replacement
The day after the operation your exercise regime begins. With the aid of a physiotherapist you will get out of bed and begin to exercise your new knee replacement. With perseverance, you should be able to climb stairs by day 2 or 3 and go home the following day. You will need to continue attending physiotherapy as an outpatient. This can be done closer to your home with one of our recommended group of physiotherapists. For most people it will take a month or so to be walking reasonably. After three months you should be able to walk well without pain, climb stairs (leading with your operated leg) and be capable of a range of movement with your new knee from 0 degrees to at least 120 degrees.
What can I do with my new knee?
It is important to remember that a unicompartmental knee replacement will not give you a normal knee, however, it will give excellent pain relief, very good function and range of movement, which will be better than a TKR. Biomechanical studies suggest a UKR allows the most normal knee function of any type of joint replacement.
You will be able to walk a good distance and play recreational sports such tennis, golf, cycle or swim. We would not recommend running after a UKR.
Lifespan of a UKR
Studies suggest that a UKR has a better than 90% chance of surviving for more than 10 years. The small amount of bone removed means that it is easy to revise it to a Total knee replacement if the UKR wears out. Revising a worn TKR is a much more complex procedure. UKR is therefore a good option for younger more active patients.
Performed by – Alastair Davidson, Jonathan Hull, Zuhair Nawaz Andrew Perry James Singleton
Sometimes arthritis of the knee in a young or middle-aged patient is best treated by an osteotomy which takes pressure off the damaged joint surface. Typically, people who have bowed legs and get more wear of the articular cartilage on the inside of the knee may benefit from an osteotomy. This is an operation that is better for younger and more active patients. The arthritis must be limited to one part of the knee only as the osteotomy takes the weight off the damaged cartilage and puts it onto good cartilage elsewhere in the joint.
Before suggesting an Osteotomy, Joint Reaction prefer to try and control your symptoms with physiotherapy, anti-inflammatory medication and, possibly, key-hole surgery. If these treatments are not successful, then an Osteotomy would be considered.
What happens at surgery?
Under general anaesthetic, an 8 cm incision is made over the upper part of the tibia (shin bone) on the inside. The bone is cut almost all the way across using X Rays to guide the cut. The alignment of the tibia is then carefully adjusted by opening this cut in the bone until the desired alignment is reached. The bone is then fixed with a plate that is held in place with screws. This is a called on opening wedge osteotomy. The triangular gap in the bone will fill in with new bone over the next few months post surgery.
After the operation
Most patients are ready to go home after 48 hours. The plate and screws are made of titanium and are very strong so you can partially bear weight on the operated leg with crutches. After six weeks, if the x-rays show the tibia is healing well you can progress to full weight bearing and dispense with your crutches as the discomfort settles.

High Tibial Osteotomy

High Tibial Osteotomy
Long term outlook
This operation is designed to improve the symptoms of knee arthritis but it cannot cure the disease. It will eventually get worse and further surgery will almost certainly be necessary. It will be necessary to remove the plate once the osteotomy has united as it will be in the way when further surgery is required in the future. This is a much smaller procedure and can be done as a day case generally about a year after the osteotomy.
Studies have shown that osteotomy can delay the need for a knee replacement for up to 10 years and this is often enough to keep the knee comfortable until, for example, the patient retires from work. The advantage over a knee replacement in the younger patient is that it does not involve placing an implant into the knee itself, and once it has healed, you can lead a busy, vigorous life, even returning to sport in some cases.
For the patient in their late fifties or early sixties, however, a unicompartmental knee replacement may be a better alternative.
Performed by – Alastair Davidson, Jonathan Hull, Zuhair Nawaz Andrew Perry, Seb Sturridge
Although the failure rate is low, knee replacements do not last forever. There are two main reasons to revise a knee replacement. Infection can cause early loosening of the TKR. This usually occurs in the first couple of years after the initial operation and is due to a low grade infection that occurs at the time of the initial surgery.
The other main reason for TKR failure is the non-infective loosening of the knee replacement. This generally occurs several years after initial operation and can be due to a mechanical failure of the knee replacement. In some early knee replacement designs, the plastic part of the tibial component became worn and failed after 8-10 years. Newer designs will last much longer and you can expect the plastic to last for 20 years, but eventually even these will show signs of wear.
What happens in Surgery?
The surgery involves removing the old knee replacement whilst leaving as much of the original bone as possible. There can be a considerable amount of bone loss, particularly if the old knee replacement has been infected. If this is the case, it may be necessary to complete the procedure with two operations. In the first, the old knee replacement is removed and the wound is closed. Then antibiotics are given and the infection eradicated over 4-6 weeks. The second stage involves the insertion of the new knee replacement. This technique minimises the risk of any further infection. If there is no infection only one operation is required.
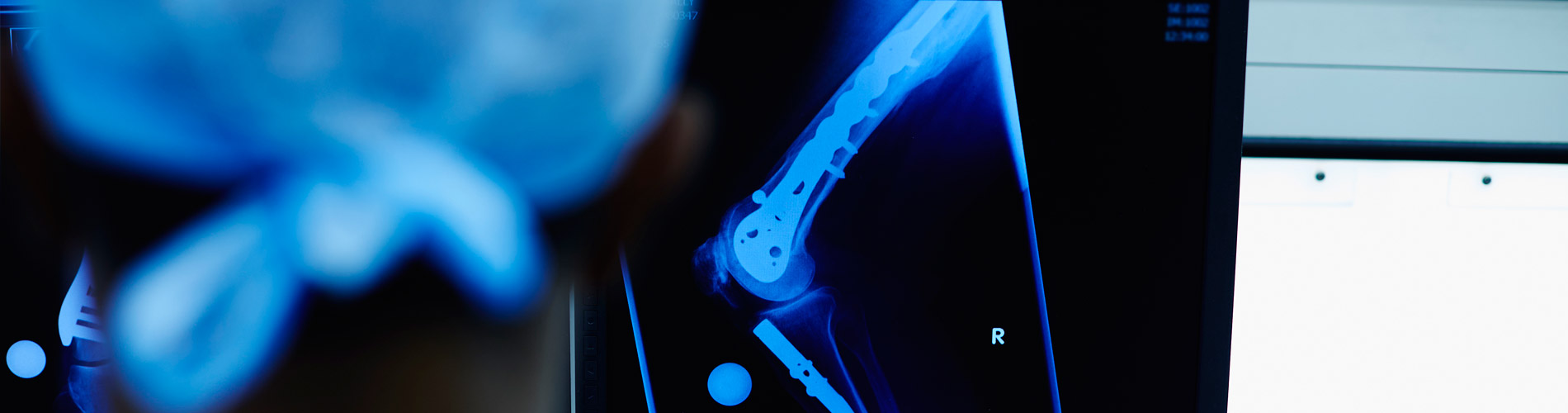
The revision TKR is similar to the Primary TKR. The revision, however, needs to be able to deal with the loss of bone incurred during the removal of the original knee replacement. This is achieved by using metal blocks and stems, which attach to the main components and compensate for any loss of bone.
The two X-ray images (1 & 2) illustrate the differences between the original and revision knee replacements.

Loose Total Knee replacement

Revision Total Knee Replacement
The day after the operation your exercise regime begins. With the aid of a physiotherapist you will get out of bed and begin to exercise your new knee replacement. With perseverance, you should be able to climb stairs by day 5 or 6 and go home the following day.
You will need to continue attending physiotherapy as an outpatient. This can be done closer to your home with one of our recommended group of physiotherapists.
For most people it will take around 6-8 weeks to be walking reasonably. After six months you should be able to walk well without pain, climb stairs (leading with your operated leg) and be capable of a range of movement with your new knee from 0 degrees to at least 90 degrees.
What can I do with my new knee?
The outcome of a revision TKR is generally not as good as that of a primary knee replacement. The revision knee replacement will, however, give excellent pain relief and as good a range of movement as a primary TKR. You will be able to walk without pain and climb stairs although you may need a stick to walk longer distances.
Lifespan of a Revision TKR
The lifespan of a revised TKR depends on the reasons for revision and the complexity of the procedure. There is a better than 80% chance that two operations for revision of an infected TKR will result in a knee replacement that is free of infection. Longevity of a revision knee replacement will be less than for a primary TKR but 80-85% should be still functioning after 10 years.
Performed by – Alastair Davidson, Jonathan Hull, Zuhair Nawaz Andrew Perry James Singleton
Patello Femoral replacement (PFA) is performed for arthritis affecting the patella, i.e. the kneecap, and the front of the knee that it rubs against as the knee bends. In about 10% of arthritis patients the majority of their knee symptoms are coming from a worn kneecap. These people suffer from pain when crouching, climbing and descending stairs, walking up slopes and getting out of low chairs. Patients with this condition are usually able to walk well on the flat and still have a good range of movement of the knee, which would be reduced with a total knee replacement. Initially Patello Femoral Arthritis can be treated with painkillers, anti-inflammatories, physiotherapy and, in the earlier stages, arthroscopy (keyhole surgery) but as the knee progressively wears, joint replacement surgery may be required to relieve the pain and improve function and mobility. If the majority of the joint is free from arthritis (or displays minimal symptoms) it may be possible to replace the back of the patella and the front of the femur (thigh bone) to provide relief. If other parts of the knee are also affected a total knee replacement is the better option.
What happens in surgery?
The surgery involves removing a small thickness of the damaged bone from the front of the femur (thigh bone) and the back of the patella (kneecap). The Patello Femoral replacement fits inside the space and is fixed to the bone with cement. The operation takes about an hour and involves a 15cm incision over the front of the knee and through the quadriceps muscle.
The component parts of the PFR
The Patello Femoral Replacement comes in two parts. The Femoral component is made of metal and is highly polished. The back of the patella is covered with a plastic button, which sits in a shallow groove on the front of the metal femoral component. Essentially a Patello Femoral Replacement is the front part of a Total Knee Replacement, but leaves the unworn cartilage over the rest of the joint intact.
After a Patello Femoral Replacement
With the aid of a physiotherapist you will get out of bed and begin to exercise your new knee replacement. With perseverance, you should be able to climb stairs by day 2 and go home on day 3, although you may need another day if still stiff. It is very important to continue attending regular physiotherapy as an outpatient as well as diligently working on your stretches and range of movement exercises at home to get the best result. This can be achieved with one of our recommended group of physiotherapists or one closer to your home. For most people it will take around 6 weeks to be walking reasonably with only one stick, at which time you can return to driving a manual car. After three months you should be able to walk well without pain, be back to normal daily activities, and be capable of a range of movement with your new knee from 0 degrees to 120 degrees. However, this range of movement may not be as good as it was before surgery and you may not be able to kneel after your Patello Femoral Replacement, although you will not damage the knee if you do. It is important to remember that an artificial knee is not a normal knee but that this will feel much more normal than a total knee replacement. You should be able to return to all your normal daily activities and sports such as golf, tennis, bowls, cycling, swimming.
Lifespan of the PFR
Studies suggest that a Patello Femoral Replacement has around an 85% probability of lasting for 10 years after surgery. It is frequently done in a younger age group, such as patient’s aged 50 or over, as it is relatively easy to convert to a TKR if it wears out. It is performed less often in older patients as they frequently have osteoarthritis that affects the rest of the knee as well, making a TKR a better option
Performed by – Alastair Davidson, Jonathan Hull, Zuhair Nawaz Andrew Perry James Singleton
he Posterior Cruciate Ligament links the tibia (shin bone) to the femur (thigh bone). It is situated in the middle of the knee and is important in controlling movement of the two bones, particularly during sport. The PCL is typically damaged during sporting activity by forcing the tibia backwards when the knee is flexed at 90 degrees.
Reconstruction of the Posterior Cruciate Ligament (PCL) of the knee is not required as often as ACL reconstruction. Usually PCL injuries do well with physiotherapy but when the knee remains unstable, an operation may be required.
Diagnosis of PCL injury
The diagnosis depends on a clinical examination at which time the laxity of the PCL and any other ligaments can be assessed. An MRI scan will also usually be done to assess the severity of the PCL injury and to see if the meniscal cartilages are also damaged. Only the more severe injuries need surgery. Partial injuries can generally be treated with physiotherapy and achieve a good functional result with return to high level sports.
What happens at surgery?
The operation requires a general or spinal anaesthetic and one night in hospital. The procedure involves excising the damaged PCL and replacing it with a graft of your own tissues. Most of the operation is done through keyholes but there is also one 3 cm incision below the knee.
The surgeons at Joint Reaction prefer to use a hamstring graft. In this technique 2 tendons from the inside of your knee are removed via a 3cm incision below the kneecap. Despite the loss of these tendons your hamstring strength will return to almost normal after rehabilitation.
The graft is inserted into the knee via tunnels drilled in the bone of the tibia and femur and is secured with screws in these tunnels.
In many cases other structures can be injured at the time of a PCL rupture. Frequently a reconstruction of the tissues on the postero lateral aspect of the knee needs to be done at the same time.
After the operation
The knee will be swollen and uncomfortable for a week or two. You will need to wear a hinged brace, which will be locked straight for the first fortnight and after that will start physiotherapy to get the knee bending. For the first month, we will recommend only passive bending (ie, with your physio carefully assisting, without you actively trying to make the knee bend). After that, from six weeks onwards, the exercises will progressively increase so that by 3 months post-op you should be walking well without help or a limp. We would not recommend any high impact sports until at least 6 months have passed.
Outcome
Because it takes more force to rupture the PCL than the ACL, and because other structures in the knee may have been damaged, the outcome from PCL reconstruction may not be as good as after ACL reconstruction. Osteoarthritis may occur and although the knee should feel stable, you may not be able to return to as vigorous sporting activity as before the injury.
Performed by – Alastair Davidson
Defects in the articular cartilage covering the bones of the knee joint can be caused by traumatic injuries as well as minor twisting injuries. They will result in pain and swelling as well as sometimes clicking and locking of the knee. These are usually first treated with knee arthroscopy (keyhole surgery) and a smoothing of the edges as well as a ‘microfracture’ to full thickness defects which involves small picks used to make holes through the surface of the bone to release the bone marrow which contains stem cells to promote healing of the cartilage that would otherwise heal poorly.
Such defects left untreated usually continue to cause pain and problems and will develop into arthritis. Further technical advances have now made it possible to fill the defects with scaffolds to enhance the result of the microfracture technique which can be further enhanced by bone marrow aspiration cells, gained through another small stab incision, to create a higher concentration of stem cells in the affected area. It is important to realise that this technique is for isolated defects surrounded by healthy cartilage, much as one repairs the divots on a golf course by patching the hole, rather than for established arthritis.
Performed by – Alastair Davidson, Zuhair Nawaz Andrew Perry James Singleton
Instability of the patella (kneecap) can present with pain or in more extreme circumstances dislocation. There are many reasons why the patella may not work well and some will require surgery to correct them.
In the first instance a careful clinical examination is required together with plain X rays and possibly an MRI scan. In some cases, a CT scan may also be required.
The majority of cases will be treated with physiotherapy in the first instance to strengthen the muscles of the thigh and improve the tracking of the patella. This will improve the symptoms in the majority of patients and apart from maintaining the muscles no further treatment is required.
In some patients there are anatomical abnormalities that mean physiotherapy is unlikely to resolve the problem. Sometimes the patella can be too high, the groove on the front of the femur (thigh bone) which the patella passes down may be too shallow, the attachment of the tendon to the front of the tibia (tibial tubercule) can be too lateral and the ligaments on the inside of the patella can be weak or damaged after a dislocation. All of these make dislocation more likely to occur in the future.
Surgical treatment will be directed at the problem or problems as more than one is frequently present.
If the patella is too high or the tibial tubercule too laterally placed, the tubercule can be moved inwards or downwards to correct the problem. This is called a tibial tubercule osteotomy.
If the ligaments on the inside of the patella are weak or damaged they can be reconstructed using a tendon graft to make them strong again. This is called a medial patella femoral ligament reconstruction.
If the groove on the front of the femur down which the patella passes is too shallow it can be deepened with a procedure called a trochleoplasty.
Patello femoral surgery
Generally, you will be in hospital overnight. The surgery is done under a general anaesthetic and local anaesthetic is injected around the wound for pain relief after the operation.
Surgery can generally be done using several; small transverse incisions, about 2cm long, which will heal better than a single vertical incision.
You will need to be in a leg immobiliser splint for a period after surgery to support the knee but in most cases you will be able to take full weight on the leg early on. Physiotherapy is very important and in most cases the leg immobiliser splint can be removed when you regain a straight leg raise, generally in 2-3 weeks. By 6 weeks you should be able to walk normally. The exception to this is surgery to move the tibial tubercule downwards when you will need a leg immobiliser splint and crutches for 6 weeks while the bone heals.

AP X Ray after surgery to reconstruct the medial patello femoral ligaments and move the tibial tubercle distally

Lateral X Ray after surgery to reconstruct the medial patello femoral ligaments and move the tibial tubercle distally







